Introduction: A brain collision tumor represents two coexisting, histologically distinct primary tumors in one and the same region. The most common type is a collision tumor comprising a meningioma and glioma. Gliomas are usually distributed at the brain periphery. Most frequently meningiomas are attached to the cerebral falx, the convexity of the dura mater, and the base of the skull, although meningiomas without dural attachment also exist. The two tumor types can occur simultaneously, or a glioma can appear after the treatment of a meningioma [3].
Diffusely infiltrating astrocytomas constitute the largest group of brain tumors and include the astrocytic tumors, most prevalent in the adult brain [7]. They are predominantly localized in the supratentorial space and exhibit unidirectional distribution more frequent in male at a mature age [8]. The areas of invaded cortex may reveal aggregation of tumor cells beneath pia mater and around the neurons, a phenomenon known as satelitosis. A complex and disorderly proliferation of blood vessels in the tumor stroma or zone of coagulative tumor necrosis in a combination of citologically malignant fibrillary astrocytic neoplasm mandate classification of the lesion as a glioblastoma [5]. Typical for glioblastoma are giant multinucleated cells with large “monstrous” nuclei. The stromal vessels show endothelial proliferations, called glomeruloids. In glioblastoma multiforme are also found serpentine shaped necrotic areas, radially covered by tumor cells. These structures are called pseudopalisades [2].
Meningiomas with brain invasion are classified as grade II neoplasms by the WHO classification, regardless of the degree of histologic anaplasia, because they recur at a rate similar to that of atypical meningiomas. The immunohistochemical examination of the tumor brain interface with Glial fibrillary acidic protein (GFAP) is very helpful to identify brain infiltration. GFAP is useful for evaluation of the first resection, because the brain tumor interface in any recurrence may be altered by surgical intervention. GFAP immunohistochemistry demonstrates incorporation of reactive brain tissue in a malignant meningioma with brain invasion [4].
Case report
Anamnesis: 57-years old woman was admitted to the Neurosurgery department complaining of persistent headache for 3-4 weeks, unstable blood pressure levels and fatigue. During the last few days the complaints became more intense. Nausea and vomiting also appeared.
Physical examination: The patient was adequate, slightly somnolent with unstable attention and left-sided hemiparesis.
Diagnostic and therapeutic procedures: The performed computed tomography of the brain and posterior cranial fossa showed evidence of a tumor formation in the right hemisphere. The formation had solid-cystic appearance and caused compression-dislocation syndrome.
Surgical intervention: Osteoclastic temporo-parietal right craniotomy was performed. After opening the dura mater with microsurgical technique was found formation with size 5,5×5 cm, which was totally extirpated. The compression and dislocation of the medial brain structures was managed. Hemostasis, plastic repair of dura mater and closing of the cranial cavity were also performed. Postoperative period was without complications. On the first day after the surgical intervention the patient quickly became contact and adequate.
Material and metods: The histologic specimens were made with 10% neutral formalin fixation and embedded in paraffin. The cut sections were 5 mkm thick and stained with hematoxylin and eosin (HЕ). An immunohistochemical investigation with GFAP was also performed.
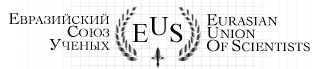
Results: The tumor formation showed areas with different macroscopic appearance. One part was grayish-pink, friable, with homogeneous cut surface. The other component was reddish-brown and elastic. The initial histological result gave different diagnoses for the histological cuts of the different tumor areas, described above: specimen № 1 — astroglial tumor grade I-II; specimen № 2 — vascular tumor of the meninges with the morphological characteristic of cavernous hemangioma. The microscopic specimens with paraffin blocks are provided for a second opinion in University Hospital «St. George «-Plovdiv. The histological specimen № 1 showed the presence of grade II astrocytoma (Fig.1).
Pathological examination after surgery, specimen № 1, H&E, magn. × 400 : Astrocytoma grade II (Fig.1).
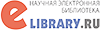
The same tumor parenchyma was found in some areas of specimen № 2, as astroglial cells were primarily fibrillary type and located around numerous thick-walled blood vessels. The morphological picture of specimen №2 leaved the impression of a benign tumor of the meninges — angiomatous meningioma or cavernous hemangioma (Fig.2).
Pathological examination after surgery, specimen № 2, H&E, magn. × 100 : „Benign meningeal tumor” (Fig.2).
An additional immunohistochemical staining for GFAP of specimen № 2 was also performed (Fig.3).
Immunohistochemical staining (GFAP) of specimen №2, magn. × 100. (Fig.3)
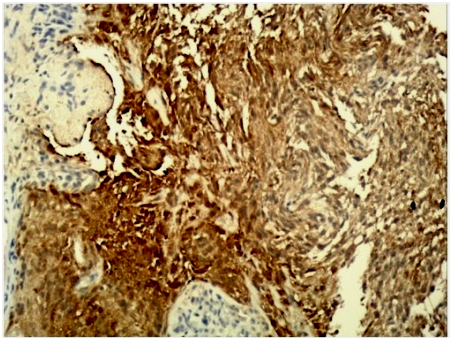
GFAP was positive in more than 85 % of the tumor cells, which supports the diagnosis of astrocytoma, superficially infiltrating the adjacent meninges.
Final diagnosis of the tumor formation: Astrocytoma grade II.
Disscusion: Aberrant angiogenesis with endothelial hyperplasia, “glomeruloids” or complex microvascular hyperplasia is a cardinal histopathologic feature for classifying a diffuse astrocytic tumor as a glioblastoma. Furthermore, anaplastic tumors have a less dense fibrillary matrix than highly differentiated astrocytomas. The majority of tumor cells demonstrate variable immunoreactivity for GFAP, confirming the astroglial nature of the tumor. Astrocytoma invasiveness is a process in progression involving adhesion, modification of the extracellular matrix and increased cellular motility. Even though astrocyte proliferation in the superficial layer of cortex may be different from conventional astrocytoma, and some cells could also be reactive, it represents the intracerebral component of these tumors. Tongues of loosely cellular and fibrillary GFAP-positive matrices extending from the cortex into leptomeninges, as well as small gemistocytes that could be followed from the cortex into leptomeninges, are in agreement with this statement [6].
Meningiomas are diverse neoplasms sharing only a tendency to arise within the histogenetically compex tissue of leptomeninges or dura mater. Brain ivasive meningiomas often reveal different from the typical appearance. The presence of brain invasion adds relatively little to the predictive power of the WHO/Mayo Clinic scheme as a prognostic model in cases of atypical or anaplastic meningiomas. Otherwise, meningothelial tumors of conventionally benign histologic aspect that infiltrate the brain tissue appear to behave much in the manner of morphologically atypical meningiomas (e.g., the tumor exhibiting 14 mitoses per 10 high-power microscopic fields, necrosis and cerebrospinal invasion) [5]. Furthermore, primary occurrence of meningiomas without dural attachment is rare. They are divided into intraventricular, in pineal region, deep sylvian, intraparenchymal/subcortical and others. Angiomatous meningioma with intraparenchymal location is extremely rare [1]. In the presented case some areas of astrocytoma grade ІІ resembled angiomatous meningioma. Meningeal origin of the tumor can be proven by immunohistochemical investigation for Vimentin (strong positive immunoreaction), EMA (immunoreaction may be weak or focal, but positive in 70% of the cases) and S-100 protein. GFAP is negative, as in the reported case.
Conclusion: Fibrillary superficial supratentorial astrocytomas histologically can resemble meningiomas. Although these two types of tumors sometimes occur simultaneously or sequentially in one and the same patient, increased caution in their clarification is needed. Their correct diagnosis requires careful consideration of the stromal vascular and fibrillary components of the tumor parenchyma. The immunohistochemical investigation with GFAP can be crucial for the diagnosis.
References:
- Banzal D., Diwaker P., Gogoi P. et al. „Intraparenchymal Angiomatous Meningioma: A Diagnostic Dilemma.”, Journal of Clinical and Diagnostic Research., DOI: 7860/JCDR/2015/15950.6602, Vol-9(10), pp 7-8, 2015.
- Bivolarski I., „Brain tumors”, https://zdrave-bg.eu/ Brain tumors /, Published July 26, 2012. Accessed October 04, 2012.
- Duoduo Z., Jinlu Y., Yunbao G. et al., „An intraventricular meningioma and recurrent astrocytoma collision tumor: a case report and literature review”, World Journal of Surgical Oncology 13:37, 2015.
- Fletcher C., „Diagnostic histopathology of tumors”, fourth edition, pp. 1936-1999,
- Rosai and Ackerman’s „Surgical Pathology”, tenth edition, vol. 2, pp. 2339-2389, 2011.
- Taratuto , Monges J., Lylyk P., Leiguarda R., „Superficial cerebral astrocytoma attached to dura report of six cases in infants”, Cancer, 54:2505-2512, 1984.
- Zaprianov Z., I. Bivolarski, G. Ivanov, D. Staikov; “Biologic parameters and their dynamics in primary and recurrent CNS tumors”. Folia Medica, XLIII, Suppl. 1:60,
- Zaprianov, Z; Bivolarski, G. Ivanov, D. Staikov; “Dynamics in frequency and distribution of central nervous system tumors in the last 50 years of XX century”. XIVth International Congress of Neuropathology, Brain pathology; 10:728. 2000.[schema type=»book» name=»ASTROCYTOMA, MIMICKING ANGIOMATOUS MENINGIOMA» description=»A brain collision tumor represents two coexisting primary tumors in one and the same region. Most commonly occurs a collision tumor comprising a meningioma and glioma. Case presentation: We report a case of a brain tumor in 57-years old woman. The initial histological analysis of the surgically removed tumor formation suggested the coexistence of angiomatous meningioma and astrocytoma collision tumor in the same patient. The subsequent careful review of the histological result with performing of immunohistochemical staining (GFAP) proved the existence of only one tumor — astrocytoma grade II. Conclusions: In addition to the coexistence of these two types of brain tumors or their consistent occurrence in the same patient, we conclude that are possible diagnostic difficulties in cases of superficial fibrillary diffuse astrocytomas and angiomatous meningiomas. The accurate diagnosis requires careful consideration of the stromal vascular and fibrillary components of tumor parenchyma. Additional immunohistochemical investigations can be crucial for the diagnosis.» author=»Bozhkova Desislava Milenova, Koleva Mariya Stoyanova, Peshev Zhivko Vladimirov» publisher=»БАСАРАНОВИЧ ЕКАТЕРИНА» pubdate=»2016-12-28″ edition=»euroasia-science.ru_26-27.02.2016_2(23)» ebook=»yes» ]