- Introduction
The Declaration of Montréal of the International Pain Summit of the International Association for the Study of Pain (IASP) recognizes the deficits in knowledge of health care professionals regarding the mechanisms and management of pain. Therefore we try to formulate our own theory for physical analgesia or analgesia based on physical modalities, traditionally applied in physical medicine and rehabilitation.
The formulation of the gate-control theory [25] for explanation of pain deposited the base of a new epoch in the development of orthodox medicine. This was the introduction of the principle of “contra-stimulation” – final effect reticence by stimulation of inhibiting systems or else, final effect stimulation by embarrassment of inhibiting systems. The science proved the existence of unsuspected reflectory relations and dependences between processes, apparently independent. There appear conditions for infringement of traditional therapeutic thinking and for formulation of a fundamentally new approach for creation of modern, or for explanation of existing anti-pain methods – from the domain of electrology, thermo and cryotherapy, manual techniques, reflexology.
- Pain
Pain is one of the most frequent sensations, formed in the nervous system, with different individual characteristics. Pain is a subjective experience, defined by nociceptive activation; by changes in sensory nerves and paths, in cerebral centers — regulators of stress, affections and motivation [30]. Different factors (physical, chemical, psychic) may influence pain sensation.
The biological significance of pain sensation is to defend the organism from noxious external influences (signal of attention). The pain informs the organism and causes a reflex defensive reaction of the individual.
Contrary to the medico-philosophical systems explaining pain by a metaphysical conflict between life and death, the French philosopher René Descartes formulates a new methodology oriented to the correct thinking and the system of knowledge. In his famous works “Discourse on the Method” (1637, in French) and “Principles of philosophy” (1644, in Latin) Descartes formulates the famous statement “Cogito ergo sum” (I think, therefore I am; or better, I am thinking, therefore I exist). In “Meditations on first philosophy” (1641,1647) he explained the idea of the rational animal, the mind – body connection and of the defensive character of pain (baby fire, boy fire), including its capacity to unchain a reflectory reaction «pulling on a thread» (fig.1).
The Holland surgeon Willem Noordenbos [28] proposed the hypothesis for the multi-synaptic transmission of pain signal (1959): “One-one synaptic transmission must be the exception rather than the rule in the nervous system. Any nerve cell located in the anterior corn . . . could hardly be expected to synapse at higher level with one such similar cell only. It will probably send ramifications to many other locations, and in turn be acted upon by the ramifications of many other cells. . Far from being a continuous chain of short neurons, these fibers must constitute links in an extremely complicated nerve net in which, within limits, everything synapses more or less with everything else.»
In 1965 the collaboration between two individual investigators – the British physiologist Patrick Wall and the Canadian psychologist Ronald Melzack, generated the theory of gate control. Their common article «Pain Mechanisms: a New Theory» in ‘Science’ [25] was qualified like «the most influential ever written in the field of pain“ (fig.2). Melzack and Wall suppose the existence of a controlling mechanism in the spinal medulla, which is closed in response to the normal stimulation of fast fibers of tactile sense, but is open if the slow fibers of pain perception transport numerous and intensive sensory signals. The gate is closed (and the pain transmission is interrupted) in case of a new stimulation of the fast fibers.
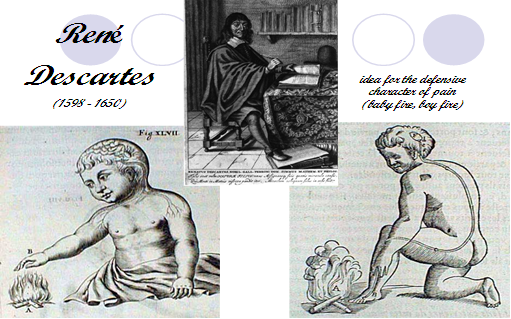
Fig.1. Rene Descartes’ ideas on pain
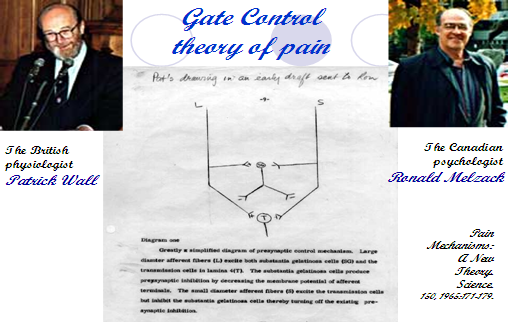
Fig.2. Gate control theory of pain
There exist different types of pain: acute and chronic (persistent) pain; nociceptive and neuropathic pain; others (central pain) [1, 2, 5, 15, 17, 26, 29, 35]. It is important to remember that the pain in clinical practice is generally combined – with nociceptive and neuropathic components, and the latter usually prevails. Some authors [32] consider that the combination of nociceptive (inflammatory hyperalgesia) and neuropathic mechanisms in every individual case is the main cause for our therapeutic helplessness, as regard pain.
In the neuropathic type of pain, the direct irritation of the nociceptor (receptor) is not necessarily present. Neuropathic pain includes mechanisms of long-time potentiation (LTP) – augmented expression of Na+, H+, Ca++ channels in the peripheral sensory nerves, generating an ectopic excitation and augmented sympathetic activity [14]. The LTP-mechanism of neuropathic pain is the theoretical base for the therapeutic use of drugs with membrane-stabilization activity, some anti-depressants and sympaticolytics [27].
Probably, preformed physical modalities execute their influence exactly on a membrane level (plasmalema and neurolema). We consider that preformed factors control the algesic type of stimulation of nociceptors (closing ion channels and thus inhibing the generation of action potentials). Presumably, peloids and physiotherapy (kinesitherapy in Bulgarian nomenclature) regulate the hyperalgesic type of stimulation (reducing the probability of irritation of nociceptors by mechanical, chemical and thermal stimulation) [21,27].
- Traditional methods for pain treatment
3.1. Medicaments [3,14, 16, 22, 32]
3.1.1. Opioid analgesics = opioids (Morphine, Codeine, Fentanyl, Meperidine, Methadone, Propoxyphene, Levorphanol, Hydromorphone, Oxycodone hydrochloride, Oxymorphone, Pentazocine) have a lot of limitations due to their side effects and the high risk of addiction.
3.1.2. Non-opioid analgesics are steroids (cortico-steroids) and non-steroidal anti-inflammatory drugs (classical NSAIDs – salycilates, diclofenac, etodolac, ibuprofen, naproxenic acid; and the modern COX-2 inhibitors – celecoxib, valdecoxib). Some authors consider acetaminophen (Tylenol, the most common antipyretic drug used in the US) as belonging to this group too. The use should be very carefully evaluated (risks of gastro-intestinal events, cardio-vascular side effects, heart failure, etc.). The dose titration is important.
3.1.3. Adjuvant analgesics are drugs that are not usually used for pain relief but may relieve pain in certain circumstances. When used to relieve pain, they are usually combined with other analgesics or non-drug pain treatments. This group includes: tricyclic antidepressants (TCAs like amitriptyline, clomipramine, desipramine, imipramine, maprotiline, nortryptyline, etc.); selective serotonin reuptake inhibitor (SSRI like fluoxetine); anticonvulsants (ACs like gabapentin, pregabaline, phenytoin, carbamazepine, clonazepam, divalproex, lamotrigine, topiramate, oxcarbazepine). The main effect of TCAs and SSRIs on pain is explained by the blockade of norepinephrine and serotonin reuptake resulting in an increased availability of these transmitters in the synapses of the descending pain-modifying pathways. The main effect of ACs on pain is explained by bind to synaptic Ca channels resulting in reduced release of neurotransmitters responsible for afferentation of pain.
3.2. Local anesthetics have different mode of application: peroral (e.g. the antiaarrhytmic Mexiletine); topical (e.g. paravertebral blockade with lidocaine); local (local injection or application of crème containing Capsaicin).
3.3. In some cases of pain (e.g. trigeminal neuralgia) local nerve destruction is applied – local injection of a nerve-destroying substance (phenol), nerve freezing by cryotherapy, nerve burning by radiotherapy.
- Actually, in physical analgesia we apply different physical modalities [4, 10, 11, 12, 13, 15, 16, 18, 19, 20, 21, 23, 24, 33, 34]:
4.1. Preformed modalities:
- Low-frequency currents and low frequency modulated middle-frequency currents (sinusoidal-modulated, interferential, Kots currents);
- Transcutaneous electroneurostimulation (TENS);
- High-frequency currents (diathermy, ultra-high frequency currents, decimeter and centimeter waves);
- Deep Oscillation (DO);
- Ultra-sound and phonophoresis with NSAIDs;
- Low-frequency magnetic field.
4.2. Natural modalities:
- Cryo-factors (ice, cold packs, cold compresses);
- Thermo-agents (hot packs, hot compresses),
- Hydro- and balneo-techniques (swilling, rubbings, showers, baths, piscine); hydro and balneo-physiotherapy techniques (underwater massage, under water exercises, etc.);
- Peloidotherapy (fango therapy, thermal mud, sea lye compresses);
- Physiotherapy techniques — stretching, post-isometric relaxation, manual therapy (traction, mobilization, manipulation); massages (manual and with devices; periostal, connective tissue massage, etc.);
4.3. Reflectory methods: electrotherapy, thermotherapy and physiotherapy in reflectory points and zones; acupuncture, laserpuncture, acupressure, etc.
- Mechanisms of physical analgesia:
5.1. In physical medicine, we applied the principles of gate-control theory of Melzack & Wall [25] for central nociceptive influence. Investigations of Gacheva [6,7,8] demonstrated that selective electrostimulation of tactile Аβ-nerve fibers (with high velocity of conduction) provokes a preliminary stimulation of suppressive neurons, that inhibit tardily occurring nociceptive stimuli of Аδ and С-fibers (with lower conduction velocity). It is assumed that a closer suppressive transfer mechanism exists at spinal level. At the peripheral level, direct anti-adaptation electrostimulation of the receptors probably provokes a hyperpolarization with an increase of the sensibility of nociceptors. A direct low frequency electrical stimulation of the Аδ and C fibers may have an analgesic effect.
5.2. We propose our own theory to explain the mechanisms of action of physical modalities on nociceptive and neuropathic pain — we introduce the notion physical analgesia or anti-pain effect of physical modalities [15,17]. The physical complexes used may provoke an analgesic effect by different mechanisms (fig.3):
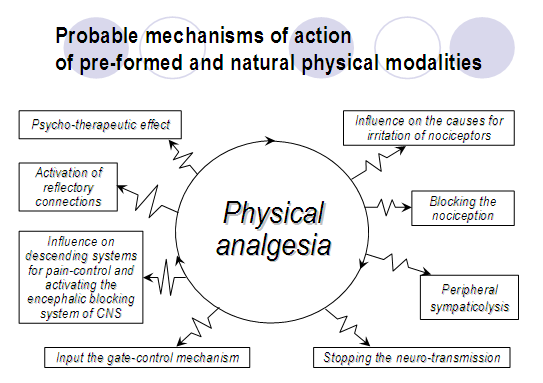
Fig.3. Mechanisms of physical analgesia
5.3. During last years, the development of physical medicine has proven the existence of some reflectory connections in the human body, based on the theory of the metameric structure of the embryo during the intra-uterine development. In physical analgesia, we apply the following groups of reflectory connections: cutaneous-visceral, subcutaneous-connective tissue-visceral, proprio-visceral, periostal-visceral and motor-visceral (Fig.4):

Fig.4. Groups of reflectory connections
5.4. The construction of a complex physical and rehabilitation programme is needed, because the mechanism of action of different procedures is diverse (Fig.5). This opinion is in agreement with modern tendencies in drug treatment of neuropathy (during the last ten years). Moreover, contemporaneous studies prescribe a combination of symptomatic and pathogenetically oriented therapy [31].
5.5. Physical modalities have an effect on the interstitium modulating the intern compartments (milieu interieur of Claude Bernard) and this way creating an optimal medium for the influence of medicament substances. This is the theoretical base for therapeutic application of a combination of drugs and physical modalities. The synergy between different physical modalities is the logical base for prescription of a complex rehabilitation program [9,15,16,17].
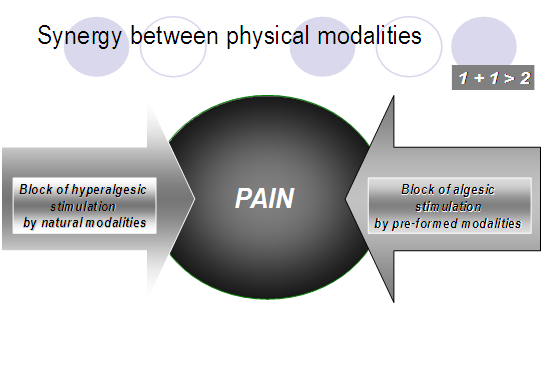
Fig.5. Synergy between physical modalities
- Conclusion
We could recommend the complex treatment of pain in rehabilitation, applying drugs and physical therapy.
The use of methods of physical analgesia in clinical practice can help to improve the quality of life of patients and to accelerate their returning to work and social activities.
Acknowledgment to the Medical University of Sofia, Bulgaria,
Via scientific Project № 34 / 2014, Contract № 50 / 2014.
References:
- Boureau F, Willer J.C., La Douleur – exploration, traitement par neurostimulation et electro-acupuncture. Paris – New York – Barcelona – Milan: Masson; 1979.
- Casey KL, editor. Pain and central nervous system diseases. The central pain syndromes. New York: Raven Press; 1992.
- Duby J.J., Campbell R.K., Setter S.M., White J.R., Rasmussen K., Diabetic neuropathy: an intensive review. Am J Health Syst Pharm. 2004;61:160-173.
- Evans R., Bronfort G., Nelson B., Goldsmith Ch., Two-Year Follow-up of a Randomized Clinical Trial of Spinal Manipulation and two types of rehabilitative exercise for Patients with Chronic Neck Pain. Spine. 2002;27(21):2383-9.
- Ferreira S.H., Prostaglandins: Peripheral and Central Analgesia. In: Bonicca JJ, editor. Advances in Pain Research and Therapy. New York: Raven Press; 1983. p.627-34.
- Gacheva J., Electrophysiological observations on ultrasound effect in some neurological diseases. Ph.D. thesis. Sofia; 1955-1960. (In Bulgarian)
- Gacheva J., Excitomotory electrodiagnostics. In: Ganev G Editor. Clinical electrophysiology. Sofia: Medizina & Fizkultura; 1970. p.193-222. (In Bulgarian)
- Gacheva J., Diagnostics and therapy with low frequency currents. Sofia: Medizina & Fizkultura; 1980. 204 p. (In Bulgarian)
- Gildenberg P.L., editor. The Chronic Pain Patient: Evaluation and Management. Vol.7 of Pain and Headache, Gildenberg – Houston – Texas Medical School; 1985. 145 p.
- Gutenbrunner C., Ward A.B., Chamberlain M.A., editors. White Book on Physical and Rehabilitation Medicine in Europe. Europa Medicophysica. 2006;42(4):289-332.
- Hayes K. Manual for physical agents. New Jersey: Prentice Hall Health; 2003. 209 p.
- Johnson M. The clinical effectiveness of TENS in pain management. Critical Reviews in Physical and Rehabilitation Medicine. 2000;12(2):131-149.
- Johnson M., Tabasam G., An investigation into the analgesic effects of different frequencies of the amplitude-modulated wave of interferential current therapy on cold-induced pain in normal subjects. Archives of Physical Medicine and Rehabilitation. 2003;84(9):1387-94.
- Kahanovitz N., Diagnosis and treatment of Low Back Pain. New York: Raven Press; 1991. 145 p.
- Koleva B., Physical analgesia and stimulation (including algorithms and methods for neurological patients). Sofia: SIMEL; 2006. 180 p. (In Bulgarian)
- Koleva I.B., Pain and physical analgesia in neurorehabilitation practice – shifting the pain management paradigm from pure pharmacological interventions. Neurorehabilitation. 2008;2(1):22-30. (In Bulgarian)
- Koleva B., Physical analgesia and Deep Oscillation. Monograph. Second Edition. Sofia: SIMEL; 2015. ISBN: 978-619-183-025-1 (In Bulgarian)
- Koleva Y.B., Yoshinov R.D., Edreva V., Kouyoumdjieva M., Examens nosometriques chez des patients lombalgiques au cours d’une cure thermale. In: Proceedings of the XI Congress of World Hydrothermal Organization. Istanbul, Turkey, 1992. P.15.
- Koleva B., Lishev N.S., Iochinov R.D., Manual-Therapeutic and Kinesitherapeutic Techniques in Patients with Cervically Related Headache. In: Proceedings of 2nd World Congress of the International Society of Physical and Rehabilitation Medicine (ISPRM), Prague, Czech Republic, 2003. P.345-350.
- Koleva B., Milanov I.G., Ioshinov R.D., Goranova Z., Complex rehabilitation in patients with tension type headache. In: Abstracts of the 36th International Danube Symposium for Neurological Sciences and Continuing Education, Sofia, 2004. p.51.
- Kotzeva , Georguiev G., Acupuncture points for influence pain. In: Shotekov P, editor. Pain – pathogenesis and treatment. Sofia: Lieder press; 1998. P.191-6. (In Bulgarian)
- Krogstad B.S., Jokstad A., Dahl B.L., Soboleva U., Somatic complaints, psychological distress, and treatment outcome in two groups of TMD patients, one previously subjected to whiplash injury. J.Orofac.Pain. 1998;12(2):136-44.
- La Freniere G., Le patient lombalgique (techniques de traitements kinésithérapeutiques). Paris – New York – Barcelona – Milan – Mexico – Sao Paulo: Masson; 1983. 194 p.
- Lewit K., Postisometric relaxation in combination with other methods of muscular facilitation and inhibition. Manual Medicine. 1986;2:101-4.
- Melzack R., Wall P., Pain mechanisms: A new theory. Science. 1965;150:971-9.
- Merskey H., Bogduk N., editors. Classification of chronic pain – descriptions of chronic pain syndromes and definition of pain terms. Seattle: IASP press; 1994.
- Nalty T., Sabbahi M., Electrotherapy Clinical Procedures Manual. Nalty T, editor. New York – St.Louis – San Francisco – Bogotá – Caracas – Lisbon – London – Madrid – Mexico City – Milan – Montréal – New Delhi – Singapore – Sydney – Tokyo — Toronto: McGraw – Hill; 2001. 299 p.
- Noordenbos W., Pain: Problems Pertaining to the Transmission of Nerve Impulses Which Give Rise to Pain. Amsterdam: Elsevier; 1959.
- Shotekov P., Anatomical and pathophysiological bases for treatment of pain. In: Shotekov P, editor. Pain – pathogenesis and treatment. Sofia: Lieder press; 1998. p.27-46. (In Bulgarian)
- Terenius L., Profiles of CSF neuropeptides in chronic pain of different nature. In: Sicuteri F, Terenius L, Vecchiet L, Maggi C, editors. Advances of pain research and therapy. 1992;20:93-100.
- Varkonyi T., Kempler P., Diabetic neuropathy: new strategies for treatment. Diabetes, obesity and metabolism. 2008;10:99-108.
- Vlaskovska M., Pharmaco-biochemical principles in pain treatment. In: Shotekov P, editor. Pain – pathogenesis and treatment. Sofia: Lieder press; 1998. 47-59. (In Bulgarian)
- Walsh D., TENS: Clinical applications and Related Therapy. Churchill Livingstone; 1997.
- Walsh M., Foster N.E., Baxter G.D., Trancutaneous electrical nerve stimulation. Relevance of stimulation parameters to neurophysiological and hypoalgesic effects. American Journal of Physical Medicine and Rehabilitation. 1995;74(3):199-206.
- Weissenberg M., Pain and pain control. In: Daitzman RJ, editor. Diagnosis and intervention in behavior therapy and behavioral medicine. Vol.1. New York: Springer; 1983. p.90-149.[schema type=»book» name=»PHYSICAL ANALGESIA OR THE POTENTIAL OF PHYSICAL MODALITIES TO REDUCE PAIN» description=»The Declaration of Montréal of the International Pain Summit of the International Association for the Study of Pain (IASP) recognizes the deficits in knowledge of health care professionals regarding the mechanisms and management of pain. Therefore we try to formulate our own theory for physical analgesia or analgesia based on physical modalities, traditionally applied in physical medicine and rehabilitation. During our modest clinical experience (of 20 years) and clinical observations and investigations on more then 2500 patients with neurological, rhumatological, orthopedical and traumatological conditions (suffering from different types of pain) we have applied differents physical factors. By our opinion the anti-pain effect of physical modalities is very important, with a high level of efficacy. Physical analgesia has not side consequences and may be applied in combination with other therapeutic factors. For physical analgesia we use: preformed modalities (electric currents, ultra-sound; magnetic field; light therapy, including laser); natural modalities (kryo-factors and thermo-agents; hydro- and balneo-techniques; peloidotherapy and physiotherapy techniques); reflectory methods. Our hypothesis is an attempt to explain pathogenetic mechanisms of physical analgesia: By influence on the cause for irritation of pain receptors — consequence of stimulation of circulation, metabolism and trophy of tissues (by low and medium frequency electric currents, magnetic field, ultrasound, He-Ne laser; massages; manual techniques); By blocking of nociception (low frequency currents, including transcutaneous electrical nerve stimulation or TENS; lasertherapy); By inhibition of peripheral senzitization (low and middle frequency currents, TENS; magnetic field; lasertherapy); By peripheral sympaticolysis (low frequency currents like dyadinamic currents, peloids); By stopping the neural transmission (by С and Аδ delta — fibers) to the body of the first neuron of the general sensibility (iontophoresis with Novocain in the receptive zone – the region of neuro-terminals); By input of the gate-control mechanism (TENS with frequency 90-130 Hz and interferential currents with high resulting frequency — 90-150 Hz); By activation of the reflectory connections: cutaneous – visceral, subcutaneous-connective tissue-visceral, proprio-visceral, periostal-visceral and motor-visceral (classic manual, connective tissue and periostal massage, post-isometric relaxation and stretching-techniques); By influence on the pain-translation in the level of posterior horn of the spinal medulla – using the root of activation of encephalic blocking system in the central nervous system (increasing the peripheral afferentation) and influence on the descending systems for pain – control (TENS with frequency 2-5 Hz and interferential currents with low resulting frequency 1-5 Hz, acupuncture and laserpuncture; reflectory and periostal massage, zonotherapy, acupressure, su-dgok massage; preformed factors in reflectory zones /palms of hands, plants of feet, paravertebral points; zones of Head, of Mackenzie, of Leube-Dicke, of Vogler-Krauss/); By inhibition of central sensitization (lasertherapy; peloidotherapy; physiotherapy); By influence on the psychic state of the patient – the drug «doctor» and the drug «procedure».» author=»Koleva Ivet Borissova, Yoshinov Borislav Radoslavov» publisher=»БАСАРАНОВИЧ ЕКАТЕРИНА» pubdate=»2017-01-09″ edition=»euroasia-science.ru_29-30.12.2015_12(21)» ebook=»yes» ]